He ʻenehana koʻikoʻi ka ERCP no ka ʻike ʻana a me ka mālama ʻana i nā maʻi biliary a me ka pancreatic. I kona puka ʻana mai, ua hāʻawi mai ia i nā manaʻo hou he nui no ka mālama ʻana i nā maʻi biliary a me ka pancreatic. ʻAʻole ia i kaupalena ʻia i ka "radiography". Ua loli ia mai ka ʻenehana diagnostic mua i kahi ʻano hou. ʻO nā ʻano hana lapaʻau e pili ana i ka sphincterotomy, ka wehe ʻana i ka pōhaku bile duct, ka hoʻokahe ʻana o ka bile a me nā ʻano hana ʻē aʻe e mālama ai i nā maʻi bile a me ka ʻōnaehana pancreatic.
Hiki i ka holomua o ka intubation bile duct koho no ERCP ke piʻi aʻe ma mua o 90%, akā aia nō kekahi mau hihia kahi e hiki ai i ke komo ʻana o ka biliary paʻakikī ke kumu o ka hāʻule ʻana o ka intubation bile duct koho. Wahi a ka ʻaelike hou loa ma ka ʻike a me ka mālama ʻana i ka ERCP, hiki ke wehewehe ʻia ka intubation paʻakikī e like me: ʻo ka manawa no ka intubation bile duct koho o ka nipple nui o ka ERCP maʻamau ʻoi aku ma mua o 10 mau minuke a i ʻole ka helu o nā hoʻāʻo intubation ʻoi aku ma mua o 5 mau manawa. I ka wā e hana ai i ka ERCP, inā paʻakikī ka intubation bile duct i kekahi mau hihia, pono e koho ʻia nā hoʻolālā kūpono i ka manawa e hoʻomaikaʻi ai i ka holomua o ka intubation bile duct. Hana kēia ʻatikala i kahi loiloi ʻōnaehana o kekahi mau ʻano hana intubation kōkua i hoʻohana ʻia e hoʻoponopono i ka intubation bile duct paʻakikī, me ka manaʻo e hāʻawi i kahi kumu kumumanaʻo no nā endoscopists lapaʻau e koho i kahi hoʻolālā pane i ka wā e kū ai i ka intubation bile duct paʻakikī no ERCP.
I.ʻO ke ʻano hana uea alakaʻi hoʻokahi, SGT
ʻO ke ʻano hana SGT ka hoʻohana ʻana i kahi catheter contrast e hoʻomau i ka hoʻāʻo ʻana e hoʻokomo i ka ʻōpū bile ma hope o ke komo ʻana o ke kaula alakaʻi i loko o ka ʻōpū pancreatic. I nā lā mua o ka hoʻomohala ʻana o ka ʻenehana ERCP, he ʻano maʻamau ka SGT no ka hoʻokomo ʻana i ka ʻōpū biliary paʻakikī. ʻO kona pono, he maʻalahi ke hana, hoʻopaʻa i ka nipple, a hiki ke noho i ka puka o ka ʻōpū pancreatic, e maʻalahi ai ka loaʻa ʻana o ka puka o ka ʻōpū bile.
Aia nā hōʻike ma nā palapala e hōʻike ana ma hope o ka hāʻule ʻana o ka intubation maʻamau, hiki i ke koho ʻana i ka intubation kōkua SGT ke hoʻopau pono i ka intubation duct bile ma kahi o 70% -80% o nā hihia. Ua kuhikuhi pū ka hōʻike i nā hihia o ka hāʻule ʻana o SGT, ʻoiai ka hoʻoponopono a me ka hoʻopili ʻana o ka pāluauea alakaʻiʻaʻole i hoʻomaikaʻi ka ʻenehana i ka holomua o ka intubation bile duct a ʻaʻole hoʻi i hoʻemi i ka nui o ka pancreatitis post-ERCP (PEP).
Ua hōʻike pū kekahi mau haʻawina ua haʻahaʻa ka nui o ka holomua o ka intubation SGT ma mua o ka pāluauea alakaʻiʻenehana a me ka ʻenehana sphincterotomy papillary transpancreatic. Ke hoʻohālikelike ʻia me nā hoʻāʻo pinepine ʻana o SGT, hoʻokō mua o ka pāluauea alakaʻihiki i ka ʻenehana a i ʻole ka ʻenehana pre-incision ke hoʻokō i nā hopena maikaʻi aʻe.
Mai ka hoʻomohala ʻana o ERCP, ua hoʻomohala ʻia nā ʻano ʻenehana hou no ka intubation paʻakikī. Ke hoʻohālikelike ʻia me ka hoʻokahiuea alakaʻiʻenehana, ʻoi aku ka maopopo o nā pono a ʻoi aku ka kiʻekiʻe o ka holomua. No laila, hoʻokahiuea alakaʻiʻAʻole hoʻohana pinepine ʻia ka ʻenehana i kēia manawa ma ke ʻano lapaʻau.
II. ʻOihana uea alakaʻi pālua,DGT
Hiki ke kapa ʻia ʻo DGT ʻo ke ʻano hana o ka uea alakaʻi duct pancreatic, ʻo ia hoʻi ke waiho ʻana i ke uea alakaʻi e komo ana i ka duct pancreatic e hahai a noho iā ia, a laila hiki ke hoʻopili hou ʻia ka uea alakaʻi ʻelua ma luna o ke uea alakaʻi duct pancreatic. Hoʻokomo ʻana i ka duct bile koho.
ʻO nā pōmaikaʻi o kēia ʻano hana:
(1) Me ke kōkua o kahiuea alakaʻi, ʻoi aku ka maʻalahi o ka loaʻa ʻana o ka wehe ʻana o ke aʻa bile, e hoʻomaʻamaʻa ana i ka intubation o ke aʻa bile;
(2) Hiki i ke kaula alakaʻi ke hoʻopaʻa i ka nipple;
(3) Ma lalo o ke alakaʻi ʻana o ka ʻauwai pancreaticuea alakaʻi, hiki ke pale ʻia ka ʻike pinepine ʻia ʻana o ke kahawai pancreatic, a laila e hōʻemi ana i ka hoʻoulu ʻana o ke kahawai pancreatic i hoʻokumu ʻia e ka intubation pinepine ʻia.
Ua ʻike ʻo Dumonceau et al. hiki ke hoʻokomo ʻia kahi uea alakaʻi a me kahi catheter ʻokoʻa i loko o ka lua biopsy i ka manawa like, a laila hōʻike i kahi hihia holomua o ke ʻano hana occupancy duct pancreatic, a hoʻoholo i kauea alakaʻiUa kūleʻa ka noho ʻana i ke ʻano hana duct pancreatic no ka intubation duct bile. He hopena maikaʻi ka helu.
Ua ʻike ʻia kahi noiʻi e pili ana i ka DGT na Liu Deren et al. ma hope o ka hana ʻia ʻana o DGT ma nā poʻe maʻi me ka paʻakikī o ka ERCP bile duct intubation, ua hōʻea ka holomua o ka intubation i 95.65%, ʻoi aku ka kiʻekiʻe ma mua o ka holomua o 59.09% o ka intubation maʻamau.
Ua kuhikuhi ʻia kahi noiʻi e hiki mai ana e Wang Fuquan et al. i ka wā i hoʻopili ʻia ai ʻo DGT i nā poʻe maʻi me ka paʻakikī o ka ERCP bile duct intubation i ka hui hoʻokolohua, ua kiʻekiʻe ka nui o ka holomua o ka intubation e like me 96.0%.
Ua hōʻike ʻia nā haʻawina i luna nei e hiki i ka hoʻopili ʻana o DGT i nā poʻe maʻi me ka paʻakikī o ka intubation bile duct no ERCP ke hoʻomaikaʻi maikaʻi i ka holomua o ka intubation bile duct.
ʻO nā hemahema o DGT e komo pū me kēia mau mea ʻelua:
(1) ʻO ka pancreasuea alakaʻimalia paha ua nalowale i ka wā o ka intubation bile duct, a i ʻole ka luauea alakaʻihiki ke komo hou i loko o ke kahawai pancreatic;
(2) ʻAʻole kūpono kēia ʻano hana no nā hihia e like me ke kanesa poʻo pancreatic, ka tortuosity o ke ala pancreatic, a me ka fission pancreatic.
Mai ka manaʻo o ka hanana PEP, ʻoi aku ka haʻahaʻa o ka hanana PEP o DGT ma mua o ka intubation bile duct maʻamau. Ua kuhikuhi kahi noiʻi e hiki mai ana he 2.38% wale nō ka hanana o PEP ma hope o DGT i nā poʻe maʻi ERCP me ka intubation bile duct paʻakikī. Kuhikuhi kekahi mau palapala ʻoiai ʻoi aku ka kiʻekiʻe o ka holomua o ka DGT i ka intubation bile duct, ʻoi aku ka kiʻekiʻe o ka hanana o ka pancreatitis post-DGT i hoʻohālikelike ʻia me nā hana hoʻoponopono ʻē aʻe, no ka mea, hiki i ka hana DGT ke hōʻino i ka pancreatic duct a me kona wehe ʻana. ʻOiai kēia, kuhikuhi mau ka manaʻo ma ka home a me nā ʻāina ʻē i nā hihia o ka intubation bile duct paʻakikī, i ka wā e paʻakikī ai ka intubation a ua hewa pinepine ka pancreatic duct, ʻo DGT ke koho mua no ka mea ʻoi aku ka liʻiliʻi o ka paʻakikī o ka ʻenehana DGT i ka hana, a maʻalahi hoʻi e kaohi. Hoʻohana nui ʻia ia i ka intubation paʻakikī koho.
III. ʻO ke alakaʻi uea cannulation-pan-creatic stent, WGC-P5
Hiki ke kapa ʻia ʻo WGC-PS ʻo ke ʻano hana o ka pancreatic duct stent. ʻO kēia ke ʻano hana e kau i ka pancreatic duct stent me kauea alakaʻii komo hewa i loko o ke kahawai pancreatic, a laila e huki i waho i kauea alakaʻia hana i ka cannulation bile duct ma luna o ka stent.
Ua hōʻike ʻia kahi noiʻi na Hakuta et al. ma waho aʻe o ka hoʻomaikaʻi ʻana i ka holomua o ka intubation holoʻokoʻa ma ke alakaʻi ʻana i ka intubation, hiki i ka WGC-PS ke pale i ka wehe ʻana o ke kahawai pancreatic a hōʻemi nui i ka hanana o PEP.
Ua kuhikuhi ʻia kahi noiʻi e pili ana i ka WGC-PS na Zou Chuanxin et al. ua hōʻea ka helu holomua o ka intubation paʻakikī me ka hoʻohana ʻana i ke ʻano hana stent occupation duct pancreatic manawa pōkole i 97.67%, a ua hoʻemi nui ʻia ka nui o ka PEP.
Ua ʻike ʻia kekahi noiʻi ke kau pono ʻia ka stent duct pancreatic, ua emi nui ka manawa kūpono o ka pancreatitis postoperative koʻikoʻi i nā hihia intubation paʻakikī.
He mau hemahema nō kēia ʻano hana. No ka laʻana, hiki ke hoʻoneʻe ʻia ka stent duct pancreatic i hoʻokomo ʻia i ka wā o ka hana ERCP; inā pono e kau ʻia ka stent no ka manawa lōʻihi ma hope o ka ERCP, e nui ka manawa e paʻa ai ka stent a me ke ālai ʻana o ka duct. ʻO ka ʻeha a me nā pilikia ʻē aʻe e alakaʻi i ka hoʻonui ʻia ʻana o ka hanana o PEP. Ua hoʻomaka mua nā ʻoihana e aʻo i nā stent duct pancreatic manawa pōkole e hiki ke neʻe koke i waho o ka duct pancreatic. ʻO ke kumu, ʻo ia ka hoʻohana ʻana i nā stent duct pancreatic e pale aku i ka PEP. Ma waho aʻe o ka hoʻemi nui ʻana i ka hanana o nā ulia PEP, hiki i kēlā mau stent ke pale aku i nā hana ʻē aʻe e wehe i ka stent a hoʻemi i ke kaumaha ma luna o nā maʻi. ʻOiai ua hōʻike nā haʻawina he hopena maikaʻi ko nā stent duct pancreatic manawa pōkole i ka hoʻemi ʻana i ka PEP, he mau palena nui ko kā lākou noi lapaʻau. No ka laʻana, i nā maʻi me nā ducts pancreatic lahilahi a me nā lālā he nui, he paʻakikī ke hoʻokomo i kahi stent duct pancreatic. E hoʻonui nui ʻia ka paʻakikī, a pono kēia hana i kahi pae ʻoihana kiʻekiʻe o nā endoscopists. He mea kūpono hoʻi ke hoʻomaopopo ʻana ʻaʻole pono e lōʻihi loa ka stent pancreatic duct i kau ʻia i loko o ka lumen duodenal. Hiki i kahi stent lōʻihi loa ke hana i ka perforation duodenal. No laila, pono e mālama pono ʻia ke koho ʻana o ke ʻano hana o ka pancreatic duct stent.
IV. ʻO ka Trans-pancreatocsphincterotomy, TPS
Hoʻohana nui ʻia ka ʻenehana TPS ma hope o ke komo hewa ʻana o ke kaula alakaʻi i loko o ke kahawai pancreatic. ʻOki ʻia ka septum ma waenakonu o ke kahawai pancreatic ma ke kuhikuhi o ke kaula alakaʻi o ke kahawai pancreatic mai ka hola 11 a i ka hola 12, a laila hoʻokomo ʻia ka ʻōmole ma ke kuhikuhi o ke kahawai bile a hiki i ke komo ʻana o ke kaula alakaʻi i loko o ke kahawai bile.
Ua hoʻohālikelike ʻia kahi noiʻi e Dai Xin et al. iā TPS a me ʻelua mau ʻenehana intubation kōkua ʻē aʻe. Hiki ke ʻike ʻia he kiʻekiʻe loa ka holomua o ka ʻenehana TPS, e hōʻea ana i ka 96.74%, akā ʻaʻole ia e hōʻike i nā hopena koʻikoʻi i hoʻohālikelike ʻia me nā ʻenehana intubation kōkua ʻelua ʻē aʻe. Nā pono.
Ua hōʻike ʻia aia nā hiʻohiʻona o ka ʻenehana TPS i kēia mau mea:
(1) He liʻiliʻi ka ʻoki no ka septum pancreaticobiliary;
(2) Haʻahaʻa ka nui o nā pilikia postoperative;
(3) He maʻalahi ke kaohi ʻana i ke koho ʻana o ke kuhikuhi ʻoki;
(4) Hiki ke hoʻohana ʻia kēia ʻano hana no nā poʻe maʻi me ka hoʻokomo hou ʻana o ka pancreatic duct a i ʻole nā nipples i loko o ka diverticulum.
Ua kuhikuhi mai nā haʻawina he nui ʻaʻole hiki i ka TPS ke hoʻomaikaʻi wale i ka holomua o ka intubation bile duct paʻakikī, akā ʻaʻole hoʻi e hoʻonui i ka nui o nā pilikia ma hope o ka ERCP. Manaʻo kekahi poʻe akamai inā hana pinepine ʻia ka intubation duct pancreatic a i ʻole ka papilla duodenal liʻiliʻi, pono e noʻonoʻo mua ʻia ka TPS. Eia nō naʻe, i ka wā e hoʻopili ai i ka TPS, pono e uku ʻia ka makaʻala i ka hiki ke stenosis duct pancreatic a me ka hoʻi hou ʻana o ka pancreatitis, ʻo ia nā pilikia lōʻihi o ka TPS.
ʻO V.Precut Sphincterotomy,PST
Hoʻohana ke ʻano hana PST i ka papillary arcuate band ma ke ʻano he palena kiʻekiʻe o ka pre-incision a me ke kuhikuhi hola 1-2 ma ke ʻano he palena e wehe ai i ka duodenal papilla sphincter e ʻike i ka wehe ʻana o ka bile a me ka pancreatic duct. Maanei, kuhikuhi pono ʻo PST i ke ʻano hana maʻamau o ka nipple sphincter pre-incision me ka hoʻohana ʻana i kahi pahi arcuate. Ma ke ʻano he hoʻolālā e hana ai me ka paʻakikī o ka intubation bile duct no ERCP, ua manaʻo nui ʻia ka ʻenehana PST ʻo ia ke koho mua no ka paʻakikī o ka intubation. ʻO ka Endoscopic nipple sphincter pre-incision e pili ana i ka endoscopic incision o ka mucosa ʻili papilla a me kahi liʻiliʻi o ka ʻiʻo sphincter ma o kahi pahi incision e ʻike i ka wehe ʻana o ka bile duct, a laila e hoʻohana i kahiuea alakaʻia i ʻole ka catheter e hoʻokomo i ka bile duct.
Ua hōʻike ʻia kahi noiʻi kūloko he kiʻekiʻe ka nui o ka holomua o PST ma 89.66%, ʻaʻole ia he ʻokoʻa nui mai DGT a me TPS. Eia nō naʻe, ʻoi aku ka kiʻekiʻe o ka hanana o PEP ma PST ma mua o DGT a me TPS.
I kēia manawa, ʻo ka hoʻoholo ʻana e hoʻohana i kēia ʻenehana e pili ana i nā kumu like ʻole. No ka laʻana, ua ʻōlelo kekahi hōʻike ʻoi aku ka maikaʻi o ka hoʻohana ʻana iā PST i nā hihia kahi i kū ʻole ai a hoʻopilikia ʻia paha ka papilla duodenal, e like me ka stenosis duodenal a i ʻole ka malignancy.
Eia kekahi, i ka hoʻohālikelike ʻia me nā hoʻolālā hoʻoponopono ʻē aʻe, ʻoi aku ka nui o nā pilikia o ka PST e like me ka PEP, a kiʻekiʻe nā koi o ke ʻoki ʻana, no laila ʻoi aku ka maikaʻi o ka hana ʻana i kēia ʻoki e nā endoscopists akamai.
VI. Papillotomy nila-pahi, NKP
He ʻano hana hoʻokomo ʻana me ke kōkua o ka pahi nila ʻo NKP. Ke paʻakikī ka hoʻokomo ʻana, hiki ke hoʻohana ʻia ka pahi nila e ʻoki i kahi ʻāpana o ka papilla a i ʻole ka sphincter mai ka puka o ka duodenal papilla ma ke kuhikuhi o ka hola 11-12, a laila e hoʻohana i kahiuea alakaʻia i ʻole ka catheter i ka hoʻokomo koho ʻana i loko o ke kahawai bile maʻamau. Ma ke ʻano he hoʻolālā hoʻoponopono no ka intubation duct bile paʻakikī, hiki i ka NKP ke hoʻomaikaʻi maikaʻi i ka holomua o ka intubation duct bile paʻakikī. I ka wā ma mua, ua manaʻo nui ʻia e hoʻonui ʻo NKP i ka nui o ka PEP i nā makahiki i hala iho nei. I nā makahiki i hala iho nei, ua kuhikuhi mai nā hōʻike loiloi retrospective he nui ʻaʻole hoʻonui ʻo NKP i ka pilikia o nā pilikia postoperative. He mea kūpono ke hoʻomaopopo ʻana inā hana ʻia ʻo NKP i ka wā mua o ka intubation paʻakikī, e kōkua nui ia e hoʻomaikaʻi i ka holomua o ka intubation. Eia nō naʻe, ʻaʻohe manaʻo like i kēia manawa i ka wā e hoʻopili ai iā NKP e hoʻokō i nā hopena maikaʻi loa. Ua hōʻike kekahi noiʻi ua hoʻopili ʻia ka nui o ka intubation o NKP i ka wāERCPʻoi aku ka kiʻekiʻe o ka helu ʻana ma lalo o 20 mau minuke ma mua o ko NKP i hoʻopili ʻia ma hope o 20 mau minuke ma hope.
ʻO nā maʻi me ka cannulation bile duct paʻakikī e pōmaikaʻi nui mai kēia ʻano hana inā he mau puʻupuʻu nipple ko lākou a i ʻole ka hoʻonui nui ʻana o ka bile duct. Eia kekahi, aia nā hōʻike e hōʻike ana i ka wā e hālāwai ai me nā hihia intubation paʻakikī, ʻoi aku ka kiʻekiʻe o ka holomua o ka hoʻohana ʻana o TPS a me NKP ma mua o ka hoʻopili wale ʻana. ʻO ka hemahema, ʻo nā ʻano hana ʻoki he nui i hoʻopili ʻia i ka nipple e hoʻonui i ka hanana o nā pilikia. No laila, pono ka noiʻi hou aku e hōʻoia inā e koho i ka pre-incision mua e hōʻemi i ka hanana o nā pilikia a i ʻole e hoʻohui i nā ana hoʻoponopono he nui e hoʻomaikaʻi i ka holomua o ka intubation paʻakikī.
VII.Fistulotomy, NKE
ʻO ke ʻano hana NKF e pili ana i ka hoʻohana ʻana i ka pahi nila e hou ai i ka mucosa ma kahi o 5mm ma luna o ka nipple, me ka hoʻohana ʻana i ke au i hui ʻia e ʻoki papa ma ka papa ma ke kuhikuhi o ka hola 11 a hiki i ka loaʻa ʻana o ke ʻano like me ka orifice a i ʻole ka bile overflow, a laila e hoʻohana i kahi uea alakaʻi e ʻike i ke kahe ʻana o ka bile a me ka ʻoki ʻana o ka ʻiʻo. Ua hana ʻia ka intubation bile duct koho ma kahi jaundice. ʻOki ka ʻoki NKF ma luna o ka puka nipple. Ma muli o ke ola ʻana o ka sinus bile duct, hoʻemi nui ia i ka pōʻino wela a me ka pōʻino mechanical i ka wehe ʻana o ka pancreatic duct, hiki ke hoʻemi i ka hanana o PEP.
Ua kuhikuhi ʻia e kahi noiʻi na Jin et al. hiki i ka holomua o ka hoʻokomo ʻana o ka ʻōmole NK ke piʻi i 96.3%, a ʻaʻohe PEP postoperative. Eia kekahi, ʻo ka holomua o NKF i ka wehe ʻana i ka pōhaku he 92.7%. No laila, ke paipai nei kēia noiʻi iā NKF ma ke ʻano he koho mua no ka wehe ʻana i ka pōhaku bile duct maʻamau. . Ke hoʻohālikelike ʻia me ka papillomyotomy maʻamau, ʻoi aku ka kiʻekiʻe o nā pilikia o ka hana NKF, a he maʻalahi ia i nā pilikia e like me ka perforation a me ke kahe ʻana o ke koko, a koi ia i ka pae hana kiʻekiʻe o nā endoscopists. Pono e aʻo mālie ʻia ke kiko wehe puka makani kūpono, ka hohonu kūpono, a me ke ʻano hana pololei.
Ke hoʻohālikelike ʻia me nā ʻano hana ʻoki mua ʻē aʻe, ʻoi aku ka maʻalahi o NKF me ka nui o ka holomua. Eia nō naʻe, pono kēia ʻano hana i ka hoʻomaʻamaʻa lōʻihi a me ka hōʻiliʻili mau ʻana e ka mea hoʻohana e mākaukau ai, no laila ʻaʻole kūpono kēia ʻano hana no nā poʻe hoʻomaka.
VIII. Hana hou-ERCP
E like me ka mea i ʻōlelo ʻia ma luna, he nui nā ala e hoʻoponopono ai i ka intubation paʻakikī. Eia nō naʻe, ʻaʻohe hōʻoia o ka holomua 100%. Ua kuhikuhi mai nā palapala pili i ka wā e paʻakikī ai ka intubation bile duct i kekahi mau hihia, ʻo ka intubation lōʻihi a me ka nui a i ʻole ka hopena thermal penetration o ka pre-cut hiki ke alakaʻi i ka edema duodenal papilla. Inā hoʻomau ka hana, ʻaʻole wale ka intubation bile duct e holomua ʻole, akā e hoʻonui pū ʻia ka manawa o nā pilikia. Inā kū mai ke kūlana ma luna, hiki iā ʻoe ke noʻonoʻo e hoʻopau i ke auERCPhana mua a hana i ka lua o ka ERCP i kahi manawa koho. Ma hope o ka nalo ʻana o ka papilloedema, e maʻalahi ka hana ERCP e hoʻokō i ka intubation holomua.
Ua hana ʻo Donnellan et al. i ka luaERCPua hana ʻia ke ʻoki ʻana ma luna o 51 mau maʻi nona ka ERCP i hāʻule ma hope o ka ʻoki mua ʻana me ka pahi nila, a ua kūleʻa 35 mau hihia, a ʻaʻole i hoʻonui ʻia ka nui o nā pilikia.
Ua hana ʻo Kim et al. i kahi hana ERCP ʻelua ma luna o 69 mau maʻi i hāʻule.ERCPma hope o ke ʻoki ʻana i ka pahi nila ma mua o ka ʻoki ʻana, a ua holomua nā hihia he 53, me ka nui o ka holomua o 76.8%. Ua hana ʻia hoʻi nā hihia i koe i kūleʻa ʻole i ke kolu o ka hana ERCP, me ka nui o ka holomua o 79.7%. , a ʻaʻole i hoʻonui nā hana he nui i ka hanana o nā pilikia.
Ua hana ʻo Yu Li et al. i nā koho kula kiʻekiʻeERCPma luna o 70 mau maʻi i hāʻule ʻole i ka ERCP ma hope o ka ʻoki mua ʻana i ka nila me ka pahi, a he 50 mau hihia i kūleʻa. Ua piʻi ka nui o ka holomua holoʻokoʻa (ERCP mua + ERCP lua) i 90.6%, a ʻaʻole i piʻi nui ka nui o nā pilikia. . ʻOiai ua hōʻoia nā hōʻike i ka pono o ka ERCP lua, ʻaʻole pono e lōʻihi loa ka manawa ma waena o ʻelua mau hana ERCP, a i kekahi mau hihia kūikawā, hiki i ka hoʻopaneʻe ʻana o ka hoʻokahe ʻana o ka biliary ke hoʻonui i ke kūlana.
IX. Hoʻokahe wai biliary i alakaʻi ʻia e ka ultrasound endoscopic, EUS-BD
He hana komohewa ka EUS-BD e hoʻohana ana i kahi nila puncture e puncture i ka gallbladder mai ka ʻōpū a i ʻole ka lumen duodenum ma lalo o ke alakaʻi ʻana o ka ultrasound, e komo i loko o ka duodenum ma o ka duodenal papilla, a laila e hana i ka intubation biliary. Hoʻokomo pū kēia ʻenehana i nā ʻano intrahepatic a me extrahepatic.
Ua hōʻike ʻia kahi noiʻi retrospective ua hōʻea ka helu holomua o EUS-BD i 82%, a ʻo ka nui o nā pilikia postoperative he 13% wale nō. Ma kahi noiʻi hoʻohālikelike, ua hoʻohālikelike ʻia ʻo EUS-BD me ka ʻenehana pre-incision, ʻoi aku ka kiʻekiʻe o kāna holomua intubation, hiki i ka 98.3%, ʻoi aku ka kiʻekiʻe ma mua o 90.3% o pre-incision. Eia nō naʻe, a hiki i kēia manawa, i hoʻohālikelike ʻia me nā ʻenehana ʻē aʻe, aia nō ka nele o ka noiʻi ʻana i ka hoʻohana ʻana o EUS no nā paʻakikī.ERCPintubation. ʻAʻole lawa ka ʻikepili e hōʻoia i ka pono o ka ʻenehana puncture duct bile i alakaʻi ʻia e EUS no nā mea paʻakikīERCPintubation. Ua hōʻike kekahi mau noiʻi ua hoʻemi ia ʻAʻole hōʻoiaʻiʻo ke kuleana o ka PEP postoperative.
X. Ka hoʻokahe ʻana o ka cholangial transhepatic percutaneous, PTCD
ʻO PTCD kekahi ʻano hana hoʻokolokolo invasive ʻē aʻe hiki ke hoʻohana ʻia me ka hui pū ʻana meERCPno ka hoʻokomo ʻana o ke ala bile paʻakikī, ʻoiai hoʻi i nā hihia o ka pale ʻana o ka biliary malignant. Hoʻohana kēia ʻenehana i kahi nila puncture e komo i loko o ke ala bile, e puncture i ke ala bile ma o ka papilla, a laila e intubate i ke ala bile retrogradely ma o kahi i mālama ʻiauea alakaʻiUa kālailai kekahi noiʻi i 47 mau maʻi me ka paʻakikī o ka intubation bile duct i hana ʻia me ke ʻano PTCD, a ua hōʻea ka helu holomua i 94%.
Ua kuhikuhi ʻia e kahi noiʻi na Yang et al. ua kaupalena ʻia ka hoʻohana ʻana o EUS-BD i ka wā e pili ana i ka stenosis hilar a me ka pono e hou i ka ʻāpana bile intrahepatic ʻākau, ʻoiai ʻo PTCD he mau pono o ka hoʻohālikelike ʻana i ke axis bile duct a ʻoi aku ka maʻalahi i nā mea alakaʻi. Pono e hoʻohana ʻia ka intubation bile duct i kēlā mau maʻi.
He hana paʻakikī ka PTCD e pono ai ke aʻo ʻōnaehana lōʻihi a me ka hoʻopau ʻana i kahi helu kūpono o nā hihia. He mea paʻakikī no nā mea hoʻomaka ke hoʻopau i kēia hana. ʻAʻole wale ka paʻakikī o ka hana ʻana i ka PTCD, akā ʻo kauea alakaʻihiki nō hoʻi ke hōʻino i ke aʻa bile i ka wā e ulu ai.
ʻOiai hiki i nā ʻano hana i luna ke hoʻomaikaʻi nui i ka holomua o ka intubation bile duct paʻakikī, pono e noʻonoʻo pono ʻia ke koho.ERCP, SGT, DGT, WGC-PS a me nā ʻano hana ʻē aʻe hiki ke noʻonoʻo ʻia; inā hāʻule nā ʻano hana i luna, hiki i nā endoscopists kiʻekiʻe a me ka ʻike ke hana i nā ʻano hana pre-incision, e like me TPS, NKP, NKF, etc.; inā mau Inā ʻaʻole hiki ke hoʻopau ʻia ka intubation bile duct koho, koho luaERCPhiki ke koho ʻia; inā ʻaʻohe o nā ʻano hana i luna e hiki ke hoʻoponopono i ka pilikia o ka intubation paʻakikī, hiki ke hoʻāʻo ʻia nā hana invasive e like me EUS-BD a me PTCD e hoʻoponopono i ka pilikia, a hiki ke koho ʻia ke ʻoki ʻana inā pono.
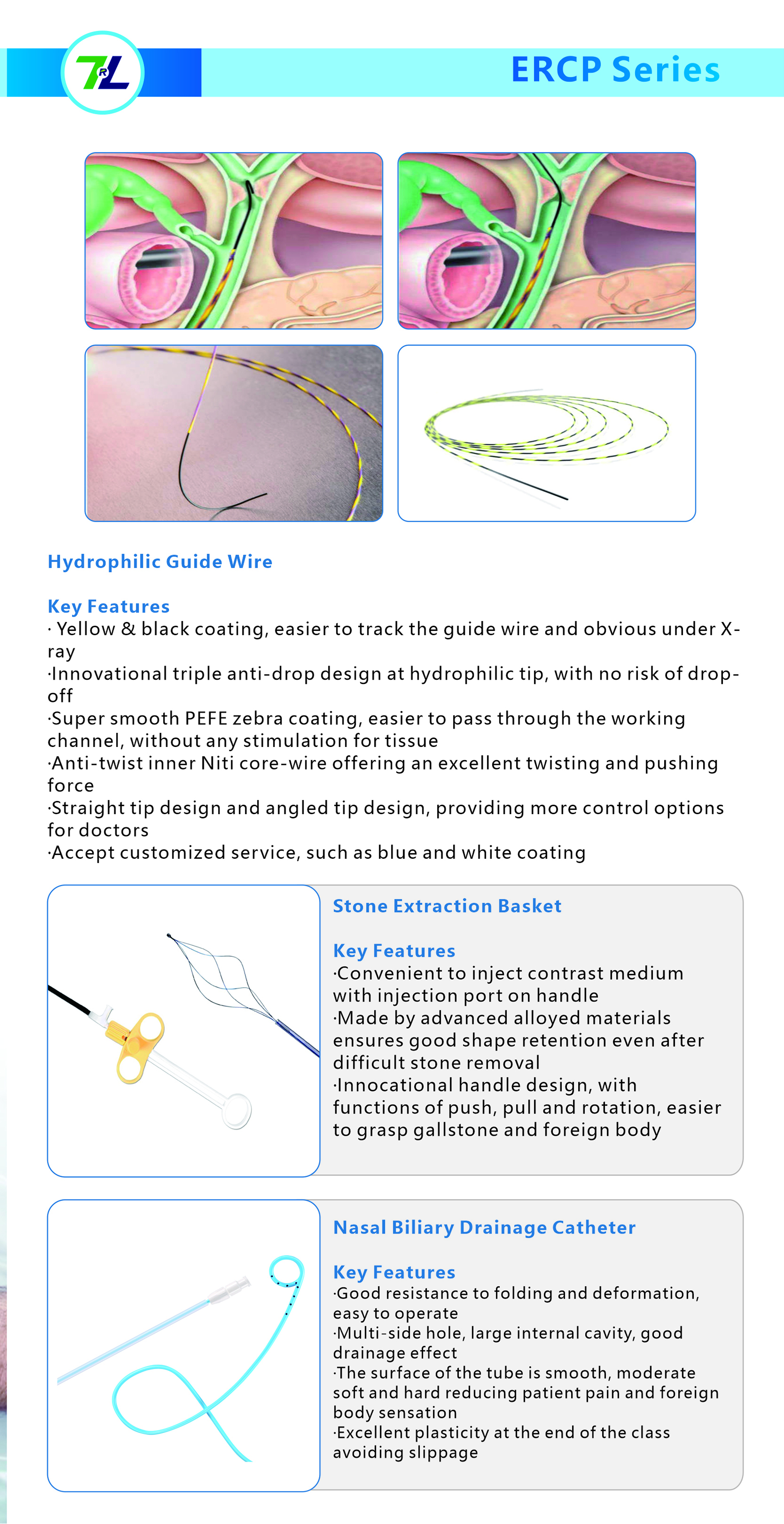
ʻO mākou, ʻo Jiangxi Zhuoruihua Medical Instrument Co., Ltd., he mea hana ma Kina e loea ana i nā mea hoʻopau endoscopic, e like me nā forceps biopsy, hemoclip, polyp snare, sclerotherapy needle, spray catheter, cytology brushes,uea alakaʻi, hīnaʻi kiʻi pōhaku, catheter hoʻokahe wai biliary ihua pēlā aku. i hoʻohana nui ʻia ma EMR, ESD,ERCPUa hōʻoia ʻia kā mākou huahana e CE, a ua hōʻoia ʻia kā mākou mau mea kanu e ISO. Ua hoʻokuʻu ʻia aku kā mākou waiwai i ʻEulopa, ʻAmelika ʻĀkau, Hikina Waena a me kekahi ʻāpana o ʻAsia, a ua loaʻa nui ka ʻike a me ka hoʻomaikaʻi ʻia e ka mea kūʻai aku!
Ka manawa hoʻouna: Ian-31-2024